FHS Covid-19 Handbook

PPE Training and Information
PPE Training
PPE TRAINING
Welcome to the Personal Protective Equipment (PPE) Training Workshop
Infection prevention and control is the first step for health and safety. Infection prevention and control (IPC) is a scientific approach and practical solution intended to prevent harm caused by infection to persons, patients and health workers. It is grounded in infectious diseases, epidemiology, social science and health system strengthening.
An important component of IPC is personal protective equipment (PPE) which is clothing or equipment designed to act as a barrier between an individual’s skin, mouth, nose, or eyes and viral and bacterial infections. Personal protective equipment (PPE) is specifically used to protect clinical and non-clinical health workers from exposure to body fluids or from droplet or airborne pathogens, chemicals or heat. The use of PPE is based on risk assessment and evidence of the route of transmission for a given microbe.
When used properly and with other infection control practices such as hand-washing, using alcohol-based hand sanitizers, and covering coughs and sneezes, PPE minimizes the spread of infection from one person to another.
All clinical sites will be providing required PPE to students. The University will provide two cloth masks (Wits logo) as well as once off, back up provision of PPE for your use in the event that you are not able to source these in your clinical sites. The Back-up PPE includes 1 box of 50 surgical masks, 1 set of goggles, 1 visor and 1 bottle of hand sanitising gel.
PPE FOR HEALTHCARE WORKERS AND STUDENTS DURING COVID-19
This poster from the NDOH demonstrates the three levels of PPE required for three levels of risk you may be exposed to when providing care for patients in the clinical settings. PPE for Low risk setting with treatment for non-COVID-19 patients is a surgical mask, no other PPE is needed. PPE for High risk settings with treatment of confirmed or presumptive COVID-19 patients is a surgical mask, apron, visor or goggles and non-sterile gloves. N95 mask is not needed unless performing aerosol-generating procedures (AGP) for confirmed or presumptive COVID-19 patients. Students are to follow these PPE guidelines along with protocols for each clinic/hospital.
I
INFECTION PREVENTION AND CONTROL
There are two main levels of IPC. 1) Standard Precautions are used for all patient care. They’re based on a risk assessment and make use of common sense practices and personal protective equipment use that protect healthcare providers from infection and prevent the spread of infection from patient to patient. 2) Transmission-Based Precautions are the second tier of basic infection control and are to be used in addition to Standard Precautions for patients who may be infected or colonized with certain infectious agents for which additional precautions, such as use of PPE, are needed to prevent infection transmission.
TRANSMISSION-BASED PRECAUTIONS OF IPC
|
IPC Measures |
Description |
Examples of PPE |
|
Contact Precautions |
Use Contact Precautions for patients with known or suspected infections that represent an increased risk for contact transmission. |
Hand hygiene, non-sterile gloves, apron/gown |
|
Droplet Precautions |
Use Droplet Precautions for patients known or suspected to be infected with pathogens transmitted by respiratory droplets that are generated by a patient who is coughing, sneezing, or talking. |
Hand hygiene, non-sterile gloves, apron/gown, surgical mask, goggles/face shield/visor |
|
Airborne Precautions |
Use Airborne Precautions for patients known or suspected to be infected with pathogens transmitted by the airborne route (e.g., tuberculosis, measles, chickenpox, disseminated herpes zoster). |
In addition to above, wear N |
CHARACTERISTICS OF SARS COV-2 IN RELATION TO IPC
Person to person transmission of SARS-CoV-2, is rapid causing large community outbreaks across the globe. The virus infects and colonises the human nasopharynx and upper respiratory tract, later affecting the lower respiratory tract leading to pneumonia, respiratory failure and sometimes death (variable case fatality rates reported 1-5%). It is an enveloped virus which makes it fragile and vulnerable to heat, chemicals and ultraviolet sunlight.
ROUTES OF TRANSMISSION OF SARS COV-2
There are only two known routes of transmission (WHO recommendations)
- Via respiratory droplets produced via sneezing, coughing which is directly inhaled person to person.
- Via respiratory droplets landing on environmental surfaces surrounding the infected person which are then transferred by the contact route via contaminated hands to a person’s face and mucous membranes.
No airborne transmission has been recorded except during aerosol generating procedures (AGP) in close proximity. In an analysis of 75,465 COVID-19 cases in China, airborne transmission was not reported.
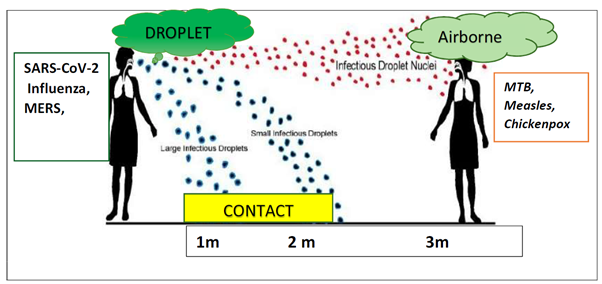
When aerosols are generated during coughing and sneezing, the larger size droplets fall on surfaces surrounding the source person depending on the mass of the droplets (See Figure below). Airborne transmission requires air currents for movement of lighter particles such as Mycobacterium tuberculosis, measles and chickenpox. This has not been found in COVID-19 transmission yet.
This is crucial information for applying the correct IPC procedures and ensuring safety of you and your patients.
IPC PRECAUTIONS FOR COVID-19 CONTAINMENT
In addition to Standard Precautions, Droplet and Contact Precautions are recommended with use of the follow PPE for contact with suspected and/or positive COVID-19 patients:
- surgical mask
- gloves non-sterile
- apron (or gown)
- goggles/face shield/visor
The National Department of Health recommends the use of N95 mask for aerosol generating procedures (AGP), protecting for airborne precautions. There is no evidence that foot or head gear is indicated for protection against droplet and contact precautions and should be avoided.
AEROSOL GENERATING PROCEDURES (AGP)
An aerosol generating procedure (AGP) is where a large number of droplets are generated during a procedure, usually relating to the mouth and respiratory tract. Currently there is no evidence that other procedures where aerosols are generated such as orthopaedics, carry a risk of transmission SARS-CoV-2.
During AGP, an N95 respirator should be worn with a gown and/ or plastic apron, single pair of nonsterile gloves and eye protection, either goggles or a face shield.
In high risk areas where AGPs are being conducted (e.g. ICU)
- Intubation, extubation and related procedures such as manual ventilation and open suctioning
- Tracheotomy/tracheostomy procedures (insertion/open suctioning/removal)
- Bronchoscopy
- Surgery and post-mortem procedures involving high-speed devices
- Some dental procedures (such as high-speed drilling)
- Non-Invasive Ventilation (NIV) such as Bi-level Positive Airway Pressure (BiPAP) and
- Continuous Positive Airway Pressure ventilation (CPAP)
- High-Frequency Oscillating Ventilation (HFOV)
- High Flow Nasal Oxygen (HFNO), also called High Flow Nasal Cannula
- Induction of sputum for laboratory test
- Collecting nasopharyngeal and oropharyngeal swabs
- Chest physiotherapy
- Reprocessing ventilator circuits and respiratory equipment
- Cardiopulmonary resuscitation, including bag-mask ventilation
PPE SUMMARY
Clinical sites are to provide appropriate PPE to all students. It is now recommended that all clinical staff and students should wear surgical masks when consulting or examining patients, irrespective whether the patient is known to have COVID-19 or respiratory symptoms. It is essential that hand hygiene is carried out before and after each patient contact.
When in contact with suspected or positive COVID-19 patients, clinical staff and students to wear: surgical mask, apron, goggles/face shield/visor and non-sterile gloves.
When performing aerosol-generating procedures, clinical staff and students to wear: N95 mask, apron or gown, goggles/face shield/visor and non-sterile gloves.
RECOMMENDED PPE FOR CLINICAL SETTING
This is a very useful chart to see what PPE is recommended for clinical staff and students in contact with patients with or without COVID-19 in different clinical settings.
EXTENDED USE OF PPE
Usually PPE is discarded after a single patient or procedure, however, because of an acute shortage of PPE during the COVID-19 outbreak, the WHO and CDC are considering extended use and/or reuse of certain PPE. For South Africa, it is recommended that the extended use of PPE is preferable. See table below
Source document: COVID-19 Disease: Infection Prevention and Control Guidelines Version 2 (21st May 2020)
Sources: CDC website, NIOH website, NICD website, NDOH website
Read the instructions for the correct sequence to put on (Don) and remove (Doff) PPE in the clinical setting.
See also PPE Training videos below for donning and doffing.